March 24, 2026 – 6:00 p.m. – 7:30 p.m. VIRTUAL
April 20, 2026 – 12:30 p.m. – 1:30 p.m. IN PERSON
May 12, 2026 – 6:00 p.m. – 7:30 p.m. VIRTUAL
Intro Block Section Instruction
Form Block Section
Write all of the introduction content below. Only use NON
FULL-WIDTH blocks.
Full-Width blocks can be inserted
outside of this block and will wrap around the form.
Use the custom HTML block below to embed your form.
Make a meaningful impact in the lives of patients.
Physician assistants play a vital role in patient care. As a PA, you’ll work closely with physicians, diagnose and treat illnesses, prescribe medications, and provide compassionate care to improve the lives of individuals and communities. Plus, with a healthcare industry shortage of primary care providers, you’ll be filling an essential role with PAs in high demand.
CASPA Application Timeframe
Open date: April 23, 2026
Deadline date: September 1, 2026
Earn a Master of Physician Assistant degree from Hardin-Simmons University and start making a difference in the health of individuals and communities across Texas and the nation. We take great pride in the many successes of our physician assistant graduates, including a 97% five-year first-time average pass rate on the National Certifying Exam (PANCE) and a 100% employment rate.
The HSU Master of Physician Assistant program has been recognized for its excellence with Accreditation-Continued status by the Accreditation Review Commission on Education for the Physician Assistant Inc. (ARC-PA). Our program stands out from other physician assistant programs around the country thanks to a balanced combination of small class sizes, hands-on learning, and a commitment to community service.
Clinical and Service-Learning Opportunities in the Master of Physician Assistant Program
Graduates from our physician assistant program have hundreds of hours of experience in clinical rotations through the following clinical experiences: family medicine, pediatrics, women’s health, mental health, internal medicine, surgery, emergency medicine, and any electives you choose to pursue. Each student will also get the chance to complete at least one clinical rotation in a rural or medically underserved area.
Our students dedicate a minimum of 50 hours to community outreach, including the chance to join our annual mission trip. In the past, physician assistant program students have traveled to Peru, the Dominican Republic, and Kenya where they had the opportunity to provide medical care to those communities. There’s no better way to begin a physician assistant career than experiencing the satisfaction of helping those in need across the world.
Jobs for Physician Assistant Program Graduates
- Emergency room physician assistant
- Surgical physician assistant
- Primary care physician assistant
- Medical specialty physician assistant
- Physician assistant educator
Why earn your Master of Physician Assistant Degree at Hardin-Simmons?
Why earn your Master of Physician Assistant Degree at Hardin-Simmons?
World-Class Physician Assistant Program Faculty
Thanks to our small student to faculty ratio (12:1), you’ll work closely with distinguished, award-winning faculty as you complete your physician assistant schooling at HSU. You’ll learn from faculty members who sit on the Texas PA board, who chair the National Exam Development Board for the PA Education Association, and who have won multiple faculty member of the year awards.
State-of-the-Art Physician Assistant Program Labs
Work and relax in our newly remodeled facilities and get hands-on experience with the tools and technology you’ll use every day in your physician assistant career. Enjoy exclusive, private 24/7 access to labs, lounges, study spaces, and a cutting-edge full-dissection cadaver lab.
Building Community
As a Master of Physician Assistant Studies student, you will join a thriving community of caring and dedicated peers and alumni. The top physician assistant careers require experience working as a team member. That’s why we encourage collaboration both inside the classroom and in the field providing healthcare to those who need it most.
Outcomes
Physician Assistants work in a variety of exciting fields of practice—including primary care, psychiatry, surgery, family medicine, and emergency medicine. Past Physician Assistant program graduates have gone on to work at prestigious facilities, such as Johns Hopkins University Medical Center, Texas Children’s Hospital, Baylor Scott & White Hospital, Covenant Hospital, and Hendrick Hospital.
After graduating from HSU’s Physician Assistant program, students are qualified to take the National Commission on Certification of Physician Assistants (NCCPA) Physician Assistant National Certifying Exam (PANCE).
On top of the personal and professional satisfaction from helping others every day, graduates also benefit from amazing job security. According to the Bureau of Labor Statistics (BLS), physician assistant career roles are expected to grow 27% over the next decade (average growth rate for all occupations is 3%). There has never been a better time to begin a physician assistant career.
Salary for Physician Assistant Program Graduates
According to the BLS, physician assistants earn an average salary of $126,000 a year.

Ben is a graduate of the Hardin-Simmons University inaugural Physician Assistant Class of 2019. Upon graduation, he started his PA career in robotic surgery at The Johns Hopkins Hospital (JHH) in Baltimore, MD where his primary responsibility is a robotics surgical PA providing specialized intraoperative assistance in robotic cases across several surgical subspecialties.
Since starting as the first and only robotics PA at JHH in 2020, Ben has grown the role into a group of PAs covering robotic cases across the department of surgery. He is the senior author on a publication in The Journal of Thoracic Cardiovascular Surgery, serves on the Education Subcommittee of the Advanced Practice Advisory Council and is a preceptor in the Surgical PA Residency Program. Ben was voted “Most Outstanding PA” by the Surgical PA Residency Cohort of 2022 and awarded “2023 APP Mentor of the Year” at JHH.
“The HSU PA Program gave me so much more than a diploma or a provider license. It gave me the rigorous training and standard to be the best provider for my future patients, while emulating the healing works of Jesus. HSU was my family while I was so far from home and friendships that will last a lifetime.”
Ben Jones

Program Details
Click on plus button at the bottom of this Accordion BLOCK (not accordion tab) to create a new tab. Select Accordion TAB block to edit tab headline. Select nested blocks within accordion tab to edit content.
-
Accrediation
The Accreditation Review Commission on Education for the Physician Assistant, Inc. (ARC-PA) has granted Accreditation-Continued status to the Hardin-Simmons University Physician Assistant Program sponsored by Hardin-Simmons University. Accreditation-Continued is an accreditation status granted when a currently accredited program complies with the ARC-PA Standards.
Accreditation remains in effect until the program closes or withdraws from the accreditation process or until accreditation is withdrawn for failure to comply with the Standards. The approximate date for the next validation review of the program by the ARC-PA will be March 2032. The review date is contingent upon continued compliance with the Accreditation Standards and ARC-PA policy.
The program’s accreditation history can be viewed on the ARC-PA website at https://www.arc-pa.org/accreditation-history-hardin-simmons-university/
-
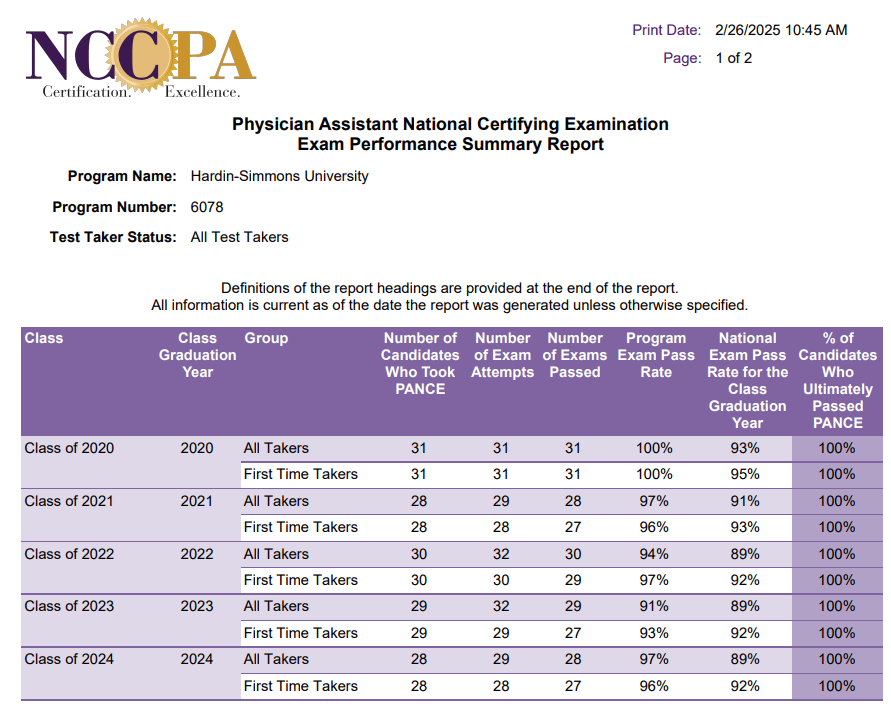
NCCPA PANCE Pass Rates
-
Physician Assistant Program Graduation Requirements
Several indicators of performance are used to determine a student’s readiness to move forward from the didactic to the clinical phase of the curriculum and to graduate from the PA program. These indicators include required courses completed; grade point average achieved; skills proficiencies attained; demonstration of professionalism; completion of 50 volunteer hours; results of comprehensive knowledge and skills testing, and completion of all requirements for the Capstone Research Project. Please refer to the student handbook for information regarding course progression and academic policy details.
Students who have been recommended for graduation by the HSU PA Program Grading and Promotions Committee will be awarded the Master of Physician Assistant degree provided they have met all of the following conditions and adhere to the policies outlined in the PA student handbook and the Hardin-Simmons University Graduate handbook.
Requirements for Graduation:
- Satisfactory completion of 21 courses during the didactic phase of the curriculum earning 53 credit hours and achieving a minimum overall 3.0-grade point average (GPA).
- Satisfactory completion of all 10 clinical rotations and three additional post-clinical courses for a total of 13 courses, earning 59 credit hours and achieving a minimum overall 3.0-grade point average (GPA).
- Satisfactory completion of three formative Objective Structured Clinical Examinations (OSCE) during the clinical phase of the curriculum.
- Documentation of competency of all required technical skills within the didactic and clinical phases of training as denoted by instructional or principal faculty.
- Satisfactory completion of course requirements for the Capstone Research project.
- Satisfactory demonstration of the ethical, professional, behavioral, and personal characteristics as documented on the professionalism evaluation forms listed below.
- End of semester professional evaluation forms during the didactic year,
- Preceptor evaluation forms during the clinical year, and
- The final summative professional assessment by the Program Director within 4 months of graduating.
- Satisfactory completion of all summative assessment components administered within 4 months before graduation from the program with a grade of 70% or greater.
- Summative OSCE,
- End of Curriculum (EOC) written examination, and
- Clinical & technical skills assessment
- Completion of a minimum of 50 hours of community service of which 20 hours must be completed by the end of the didactic year.
- Completion of a diploma card with the Hardin-Simmons University Registrar’s office.
- Satisfactory payment of all fees due to the University and meets all requirements for commencement per University policy.
- Completed any terms of Academic Probation and/or Remediation if applicable.
Students unable to fulfill these requirements by the day of graduation will not be allowed to participate in the commencement ceremony without the permission of the PA Program Director. Students will not be considered graduates in any capacity until they have completed all of the above requirements.
-
Mission Statement
The Hardin-Simmons University physician assistant program is dedicated to academic excellence in medical education. Our mission is to develop and prepare compassionate, professional PA providers who are committed to life-long leadership, learning, and community service. Our graduates will work as part of the healthcare team to deliver exceptional healthcare to rural West Texas and under-served communities worldwide.
-
Physician Assistant Program Goals
- Recruit outstanding PA students that display a commitment to community service.
- Prepare PA students for the practice of medicine as exemplified by:
- Pass rate on National Certifying exam that exceeds national average.
- Attainment of employment after graduation.
- Provide training opportunities for PA students in rural and underserved medical settings.
Progress Towards Goals Achievement
GOAL #1
- Recruit outstanding PA students that display a commitment to community service.
The following is data on the recruitment of outstanding PA students and their commitment to community service.
Overall GPA AVG Overall Science GPA AVG Written GRE Score AVG Verbal GRE Score AVG Quant GRE Score AVG Average Pre-Admission Volunteer Hours Class of 2022 3.58 3.45 4.02 153.17 152.33 591 Class of 2023 3.67 3.59 4.02 153 152.06 479 Class of 2024 3.64 3.54 4.15 153.29 153.19 373 Class of 2025 3.69 3.61 3.90 151.00 150.13 773 Class of 2026 3.68 3.62 4.17 152.00 152.83 335 Average: 3.65 3.56 4.05 152.49 152.11 510.20 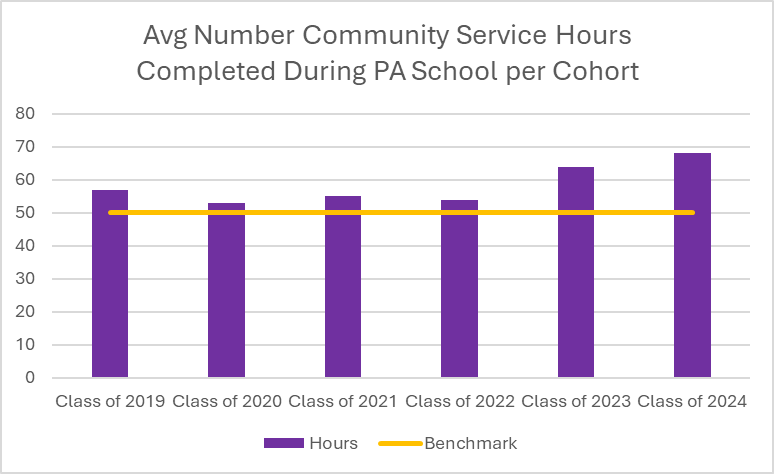
*Note all students must complete a minimum of 50 hours of community service during enrollment at the HSU PA program.
GOAL #2
- Prepare PA students for the practice of medicine as exemplified by:
- Pass rate on National Certifying exam that exceeds national average.
The first five graduating cohorts have exceeded the national average on the national certifying examination, and the HSU PA program has a five-year first-time taker average pass rate of 97% which exceeds the national five-year first-time average rate of 93%.
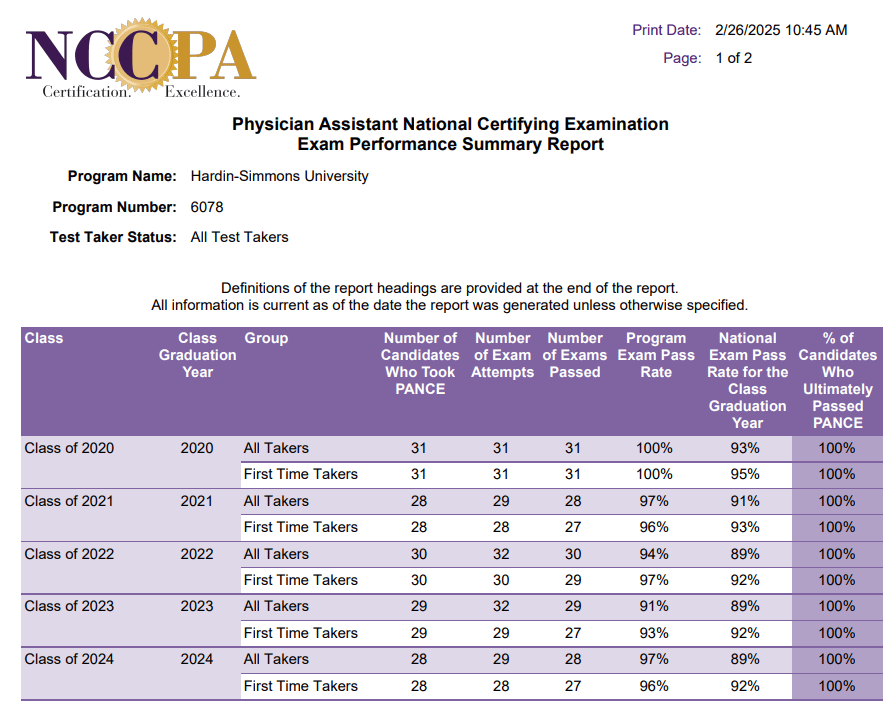
Full NCCPA 5-Year First Time Taker Summary Report
- Prepare PA students for the practice of medicine as exemplified by:
- Attainment of employment after graduation.
Class of 2019 Class of 2020 Class of 2021 Class of 2022 Class of 2023 Percentage of graduates employed* 100% 100% 100% 100% 100% *Percentage based on survey results of graduates desiring employment. Data verified with follow-up.
GOAL #3
- Provide training opportunities for PA students in rural and underserved medical settings.
Every PA student is required to complete a minimum of one clinical rotation in a rural or medically underserved area. Below is a tabular graphic demonstrating the number of clinical rotations completed in rural and underserved areas per cohort.
Clinical Rotations in Rural or Underserved Area Class of 2019 Class of 2020 Class of 2021 Class of 2022 Class of 2023 Class of 2024 Number of students 29 31 27 30 29 28 Minimum number or rotations in rural /
underserved area29 31 27 30 29 28 Additional rotations completed in rural /
underserved area26 46 37 39 14 77 Percentage above minimum goal 90% 148% 137% 130% 52% 275% Every cohort has exceeded the minimum requirement thereby allowing our students to have the opportunity to learn in rural and underserved communities.
-
Physician Assistant Program Student Attrition
HSU PA Student Attrition Table
Graduated Classes Class of 2019 Class of 2020 Class of 2021 Class of 2022 Class of 2023 Class of 2024 Maximum entering class size (as appropriately approved by ARC-PA) 30 30 30 30 30 30 Entering class size 30 31 30 30 31 31 Graduates 29 31 28 27 29 28 *Attrition rate 3.00% 0.00% 6.67% 10.00% 3.33% 9.68% **Graduation rate 96.67% 100.00% 93.33% 90.00% 96.67% 90.32% *Attrition rate calculation: Number of students who attritted from cohort divided by the entering class size.
**Graduation rate: Number of cohort graduates divided by the entering class size. -
Admissions Requirements
Applications are accepted by applying to CASPA (Centralized Application Service for Physician Assistants). A new class begins each fall semester in August. Prerequisites must be completed prior to matriculation.
Prerequisite Course Requirements+ Hours Human Anatomy with lab* 4 Human Physiology with lab* 4 *Human Anatomy & Physiology I & II with lab may be substituted (should be taken at the same institution). Biology with lab (2 separate courses) 8 Chemistry with lab 4 English 3 Microbiology with lab 4 Organic Chemistry with lab 4 Psychology 3 Sociology or an additional Psychology course 3 Statistics or Biostatistics 3 +All prerequisites must be earned from a regionally accredited U.S. college or university.
Applicants must earn a grade of C or better in all prerequisite coursework before starting the program.Other Requirements Bachelor’s degree or higher from a regionally accredited college or university Overall GPA minimum (as calculated by CASPA) 3.0 Overall Science GPA minimum (as calculated by CASPA) 3.0 Letters of Recommendation Minimum of 3 Beginning with the 2024-2025 application cycle, all applicants to the Hardin-Simmons University Physician Assistant program are encouraged to take the Physician Assistant College Admission Test (PA-CAT). The PA-CAT is a 240-item assessment covering nine (9) science subject areas. Currently, the test results are not used for admission decision-making, instead the program is collecting data on how best to implement score results to use in our admission process. Additional information on the PA-CAT can be found at https://www.pa-cat.com/
Beginning with the 2024-2025 application cycle, the Hardin-Simmons University Physician Assistant program no longer requires the GRE.
Applicant Selection Factors
Below are the application selection factors for applicants to the Hardin-Simmons University Physician Assistant program. Outstanding performance in any one category does not guarantee an interview nor does it guarantee acceptance into the program.
Application Review
In reviewing applications for interview selection and acceptance, a holistic review process is utilized that evaluates multiple factors to examine and evaluate qualities that an applicant could bring to the program.
Those factors include:
- Academic performance
- Overall GPA as calculated by CASPA
- Science GPA as calculated by CASPA
- Healthcare Experience
- Volunteer Hours
- PA Shadowing Hours
- Personal Statement
- Letters of Recommendation
Interview Review
At the interview, candidates will be evaluated on skills most likely to make them successful PA students including communication, professionalism, leadership potential, readiness to enter graduate school, problem solving, and knowledge of the profession.
Admission and enrollment practices that favor specified individuals or groups:
As noted in the FAQ section, HSU alumni and currently enrolled degree-seeking students who meet published requirements are granted an automatic interview; however, an automatic interview does not guarantee selection or favor an individual for admission beyond the interview stage.
Equal Opportunity
The Hardin-Simmons University Physician Assistant program welcomes applications regardless of race, color, national origin, religion, sex, or age. Our commitment to equal opportunity includes nondiscrimination on the basis of sexual orientation.
- Academic performance
-
Frequently Asked Questions
What is Hardin-Simmons University’s program accreditation status?
The Accreditation Review Commission on Education for the Physician Assistant, Inc. (ARC-PA) has granted Accreditation-Continued status to the Hardin-Simmons University Physician Assistant Program sponsored by Hardin-Simmons University. Accreditation-Continued is an accreditation status granted when a currently accredited program is in compliance with the ARC-PA Standards.
Accreditation remains in effect until the program closes or withdraws from the accreditation process or until accreditation is withdrawn for failure to comply with the Standards. The approximate date for the next validation review of the program by the ARC-PA will be March 2032. The review date is contingent upon continued compliance with the Accreditation Standards and ARC-PA policy.
The program’s accreditation history can be viewed on the ARC-PA website at https://www.arc-pa.org/wp-content/uploads/2023/08/Accreditation-History-Hardin-Simmons-U-272.pdf
How long is the Hardin-Simmons University Physician Assistant program?
The Hardin-Simmons Physician Assistant Program is a 27-month in-person program.Does Hardin-Simmons University have a supplemental application or supplemental fee?
HSU does not require either a supplemental application or a supplemental fee.Does HSU have Rolling Admissions, and what does that mean?
Yes, HSU does have a rolling admission process. Rolling admissions means that interviews are being conducted and admission decisions are being made while applications are still being accepted.When do most applicants submit their applications?
The CASPA application cycle opens in April. We do not review applications until verified by CASPA. All applications must be listed as “verified” in CASPA by the program’s deadline of Sept. 1 to be considered.How do I know if my courses meet the program’s prerequisite criteria?
Transcripts or planned coursework will not be reviewed for course equivalency prior to or during the CASPA application process. Guidance on prerequisites will not be provided until all prerequisites have been reviewed following the interview.Is there a preference for residents of the state of Texas?
No. Hardin-Simmons University is a private university, and no preference is given for applicants residing in the state of Texas. Tuition for the PA Program is the same for in-state and out-of-state students.Do students from HSU or others receive special consideration?
Yes – Current HSU degree-seeking students or HSU alumni receive an automatic interview if they meet the minimum criteria. Note that an interview does not guarantee acceptance.How are the interviews conducted?
Interviews for the HSU PA Program are conducted in person on campus in Abilene, TX. We do not offer virtual or video-based interviews for admission into the program. The interviews consist of an individual interview with at least one faculty member and a moderated group interview.
What are the factors that affect your admissions decisions?
We consider the following factors in making admission decisions: academic performance, cumulative grade point average (GPA), science grade point average (GPA), clinical experience (including level of responsibility and number of hours), PA shadowing experience, personal statement, reference letters, volunteer hours, fit with HSU’s mission, leadership, and interview performance.How can I make my application stand out from the rest?
Applications are holistically reviewed, meaning all elements are considered for eligible applications that meet our minimum overall CASPA calculated GPA requirement of at least a 3.0 and a CASPA calculated Science GPA of 3.0. In addition to previous academic performance and pre-admission clinical experience, these include personal statements, letters of recommendation, PA shadowing experience, volunteer or community service, leadership experience, challenging course work, academic performance, and fit with HSU mission. Competitive applicants stand out by being able to speak to each of these categories.Does it matter what your academic major is from undergrad?
No. Applications are reviewed holistically, and no specific academic major is preferred from undergraduate or graduate school experiences.Can I send additional letters of recommendation beyond those included in CASPA?
No, only three letters of recommendation included in the CASPA application submission are required. Additional letters of recommendation sent directly to the program will not be considered as part of your application.Who are members of the Admissions Committee, and who makes the final decision?
The Admissions Committee consists of the PA program faculty and staff. Final admission decisions are made by the PA Program Director and PA program faculty.Is the GRE required or accepted?
As of the 2024-2025 admission cycle, the HSU PA program no longer requires the GRE. We also are not accepting GRE score submissions as they are not considered in the admission decision-making process.
Is the PA-CAT required?
As of the 2024-2025 application cycle, all applicants to the Hardin-Simmons University Physician Assistant program are encouraged to take the Physician Assistant College Admission Test (PA-CAT). The PA-CAT is a 240-item assessment covering nine (9) science subject areas. Currently, the test results are not used for admission decision-making, instead the program is collecting data on how best to implement score results to use in our admission process. Additional information on the PA-CAT can be found at https://www.pa-cat.com/
Can I apply before I complete all the prerequisites?
Yes. When completing your CASPA application, include courses in progress and coursework planned in the appropriate fields to alert us to your plans. If you are accepted into the Program before you complete the required coursework, your acceptance will be on provisional status until records of your coursework and/or graduation are received. No student will be allowed to matriculate into the Program if prerequisite requirements are not met.Can I apply if I have not yet completed my undergraduate degree?
Yes. You can begin to apply the year prior to graduation, if you successfully graduate by the time of the PA program’s start date in August. You must have obtained your bachelor’s degree prior to matriculation into the program and completed all prerequisite coursework successfully.If I took a prerequisite course 5, 10, or even 35 years ago, would you still accept that?
Yes. We do not impose an expiration date on prerequisite coursework.Does the HSU PA Program accept prerequisites from community colleges?
Yes. We accept prerequisites from a regionally accredited institution of higher learning.Does the HSU PA Program accept prerequisite online classes and labs?
Yes. If online classes/labs are from any regionally accredited college/university.Will PASS/FAIL prerequisites be accepted when I apply?
If your PASS/FAIL course was taken during the COVID-19 pandemic (during the calendar year 2020 and 2021), it will be accepted as a prerequisite; however, the grade will not be factored into your GPA. PASS/FAIL courses taken outside of the COVID-19 pandemic dates listed above will not be accepted.Can prerequisites be waived or tested out of with CME or CEU credit?
Prerequisites cannot be waived for the Hardin-Simmons University PA Program. No prerequisite can be waived due to previous academic, life, or field experiences. Prerequisites can be completed at any regionally accredited institution of higher learning. College credit must be earned and displayed on transcripts for prerequisites. Prerequisites cannot be satisfied through Continuing Medical Education or Continuing Education Unit credit.What is your policy regarding advanced placement in PA school?
Hardin-Simmons University PA Program does not grant advanced placement in their PA Program to any matriculating student. No previous coursework will substitute for any PA courses, and the program must be completed in totality.Does the HSU PA Program accept AP or CLEP for prerequisites?
Yes. If a regionally accredited undergraduate college/university has granted AP or CLEP credit for a prerequisite course and it is displayed on the student’s transcript.Is a background check required?
Yes. Accepted students are subject to a criminal background check and drug screen preceding orientation. Should the background check or drug screen yield any undisclosed and/or disqualifying information, the offer of admission may be revoked.Do you accept transfer students or provide credit for experiential learning?
No. The PA Program does not accept transfer students from other PA Programs, and all students must have a bachelor’s degree or higher from a regionally accredited college or university in the United States before starting the PA Program. The PA Program does not allow course credit for experiential learning.Is there a minimum required number of hours for Patient Care Experience or Health Related Experience, and what’s the best way to categorize and represent my experiences?
The Hardin-Simmons University PA Program welcomes all types of experience and does not require a minimum number of hours in either patient care or health-related roles.
- Health-Related Experience typically involves non-clinical duties in a healthcare setting—such as office administration or medical scribing—where you don’t have direct patient contact.
- Patient Care Experience refers to hands-on roles that include physical assessment or direct contact with patients – such as medical assistant, nursing, phlebotomy, CNA, etc.
Deciding where to categorize each role on your application is up to you. Please contact CASPA for further guidance. We review every application holistically and value both experience types equally. Please refrain from listing the same position in both categories, as this may be perceived as fraudulent.
How should Volunteer hours be entered if they are Patient Care Experience?
Please follow CASPA’s directions on how/where to list experiences. We discourage applicants from listing the same experience in two categories as this can be viewed as fraudulent.Does the PA Program offer applicants assistance in finding clinical work or shadowing experience?
No, due to a high volume of applicants, we cannot offer assistance to candidates looking for clinical or shadowing experience.Once I submit all my application materials, how long before I hear if I will receive an interview?
The HSU PA program uses a rolling admission process without a specific timeline for notification.Can I send my application materials directly to the program?
No. All application materials must be submitted directly through CASPA. Contact CASPA at CASPA@PAEAonline.org or view the website https://paeaonline.org/resources/member-resources/caspa for questions regarding their application process. Documents sent directly to the HSU PA program will not be accepted or reviewed.Where are clinical rotation sites located?
We offer our students a wide variety of experiences in various types of clinical settings, including hospitals, small and medium-sized clinics, private offices, and rural opportunities. Our clinical team assigns those locations with input from each accepted student. Clinical rotation assignments are subject to availability at the time of assignment.What is the cost of tuition?
Tuition and fees for the PA Program is updated on the HSU PA web page yearly under the “Tuition and Fees” tab at the bottom of the page.After graduating from this program, will I be able to work in Texas or other U.S. states?
Graduation from this accredited program allows you to apply for licensure in all 50 states and allows graduates to sit for the national certification examination (required passage for licensure in most states). Each state has different licensure requirements.Are there scholarships I can apply for?
Once an applicant has been accepted into the program and is officially a Hardin-Simmons University student, they may apply for available institutional scholarships through Scholarship Central at https://hsutx.scholarshipuniverse.com/ using their official HSU student account login information. Additionally, the Chair of the PA Program Scholarship Committee will notify students as soon as any internal PA Program scholarships become available. The HSU PA program has recently received a $2 million endowment dedicated to supporting and empowering future generations of physician assistant students. This significant contribution will not only enhance our student’s education, but will also ensure the continued excellence and advancement of the Physician Assistant program at HSU.Will international coursework meet the prerequisite criteria?
Only coursework earned from a regionally accredited U.S. college or university will be accepted as prerequisite application requirements. Listed below are the 7 USDE-recognized regional accreditation agencies.
Are international students able to apply for admission into the HSU PA Program?
There are no restrictions on international students or those who have VISA status to apply to the HSU PA Program. We recommend that students contact the Financial Aid department to determine individual eligibility regarding federal funding to attend the HSU PA Program. To attend the HSU PA Program, a bachelor’s or master’s degree must be obtained from a regionally accredited institution. Please see the above FAQ in regards to pre-requisite degree requirements.
Use the following links to verify if the institution you attended (bachelor’s degree or higher) is a regionally accredited college or university:
- For applicants with multiple degrees, at least a bachelor’s degree or higher must be from a regionally accredited college or university.
- Middle States Commission of Higher Education (MSCHE)
- New England Association of Schools and Colleges, Commission on Institutions of Higher Education (NEASC-CIHE)
- The Higher Learning Commission (HLC)
- Northwest Commission on Colleges and Universities (NWCCU)
- Southern Association of Colleges and Schools Commission on Colleges (SACS)
- The Accrediting Commission for Community and Junior Colleges, Western Association of Schools and Colleges (ACCJC)
- WASC Senior College and University Commission
What are the statistics for recently admitted students?
Overall GPA AVG Overall Science GPA AVG Overall Non-Science GPA AVG Quant GRE Score AVG Written GRE Score AVG Verbal GRE Score AVG Average Pre-Admission Volunteer Hours Class of 2019 3.60 3.50 3.72 152.90 3.87 152.00 277 Class of 2020 3.65 3.63 3.67 151.77 3.95 153.23 592 Class of 2021 3.71 3.65 3.65 153.14 4.03 154.00 434 Class of 2022 3.58 3.45 3.71 152.33 4.02 153.17 591 Class of 2023 3.67 3.61 3.75 151.41 4.02 152.55 479 Class of 2024 3.64 3.54 3.77 153.19 4.15 153.29 373 Class of 2025 3.69 3.61 3.77 150.13 3.90 151.00 773 Average: 3.65 3.57 3.72 152.12 3.99 152.75 502.71 **Meeting the minimum requirements or exceeding above-average admission data does not guarantee admission, nor does it guarantee an interview.
-
Technical Standards
In order to ensure that patients receive the best medical care possible, the faculty has identified certain skills and professional behaviors that are essential for the successful progression of PA students in the Program. A student must possess skills and behaviors at a level of capability to perform a variety of duties required of a PA as a healthcare professional. Students with disabilities who can perform these skills and successfully execute professional behavior either unassisted, with dependable use of assistive devices, or by employing other reasonable accommodations are eligible to apply for enrollment in the Program.
Minimum performance standards include critical thinking, communication skills, observation skills, motor skills, and interpersonal abilities. The following descriptions define the capabilities that are necessary for an individual to successfully complete the Hardin-Simmons University Physician Assistant curriculum.
Intellectual Capability/Critical Thinking: The PA student must possess the intellectual, ethical, physical, and emotional capabilities required to undertake the full curriculum and to achieve the levels of competence in critical thinking and problem-solving required to seek entry to the profession. The ability to solve problems, a skill that is critical to the practice of medicine, requires the intellectual abilities of measurement, calculation, reasoning, analysis, and synthesis. Students in the Program must be able to demonstrate these skills in working with patients, their families, and other members of the healthcare team. Intellectual abilities also encompass learning and retaining information and the ability to make decisions in a timely manner.
Communication Skills: The PA student must be able to effectively speak, hear, and observe patients in order to elicit information, describe changes in mood, activity, and posture, and perceive nonverbal communication. The student must be able to communicate attentively, effectively, sensitively, and efficiently in oral, written, and electronic forms with other clinicians, families, and patients in order to make appropriate and timely responses.
Observation Skills: The PA student must be able to observe a patient accurately, both at a distance and close at hand. Students must possess sufficient visual, auditory, and tactile sensation to receive appropriate information in the classroom, laboratory, and other educational and clinical settings. Sensation must be satisfactory to receive verbal and nonverbal communications from patients and others and to perform inspection, auscultation, and palpation techniques during the physical examination.
Motor Skills: The PA student should have sufficient strength and coordination to perform the activities required of a Physician Assistant. The student should have sufficient motor coordination to move about patient care environments and sufficient dexterity to use common medical instruments. Students must have sufficient stamina to sit, stand, and move in classroom, laboratory, examination rooms, treatment rooms, and operating rooms for long periods of time. Students must also be able to calibrate and use large and small equipment and execute movements required for moving patients, positioning patients, and providing care to patients routinely and in emergency settings. The typical lifting requirement is a minimum of 50 lbs. unassisted.
Interpersonal Abilities: The PA student must possess the ability to establish and maintain appropriate professional relationships. The student must possess the emotional health required for full utilization of his or her intellectual abilities, the exercise of good judgment, the prompt completion of all responsibilities required for the diagnosis and care of patients, to be compassionate, empathetic, responsible, and tolerant toward patients, families, and colleagues. This also includes the ability to prioritize competing demands and function in stressful circumstances.
-
Preceptor Information
Preceptor FAQs
- What is the length or number of hours the student would be at our facility?
Each student clinical rotation is a 5-week rotation. The student schedule (days, hours, shifts, etc.) is dependent on the provider’s schedule for the 5-week duration.
- When can I expect the student to rotate at my clinical site?
The HSU PA Clinical Coordinator works closely with all preceptors and clinical sites to determine the best time to place a student. Clinical rotations are scheduled as 5-week date ranges, with clinical preceptors selecting the date ranges that best fit their schedules. If at any time the provider is unable to take a student at a previously scheduled time, please notify the program as soon as possible so alternative placements can be made.
- What are the required documents to be a clinical preceptor?
Prior to placing a student at a clinical site, an active affiliation agreement between the HSU PA program and the facility must be in place. Here is a sample affiliation agreement. If it is a group practice/site, the affiliation will be with that group. If it is a private practice, the affiliation will be with the practice. If the provider provides care at a local hospital(s), we also require an affiliation agreement to be in place with the hospital(s). HSU utilizes a standard affiliation agreement for all clinical sites, but if the partnering facility has one, we are happy to review it to determine if it will satisfy all our requirements.
In addition, a Letter of Intent is needed from the provider (provided by the HSU PA program). Please note a Letter of Intent does not oblige the provider to take students, it only notifies us of your interest.
Finally, all clinical preceptors must provide a copy of their current curriculum vitae (CV) or resume, a copy of their board certification, and a copy of their current license.
- Will PA students need access to our patient charts?
Yes, students will need access to patient charts because they will be seeing patients during their rotations. This can be electronic and/or paper. All students will have completed extensive training in HIPAA compliance prior to starting their clinical year.
- Upon completion of the student’s rotation, what is required from the preceptor?
Halfway through the clinical rotation, we ask each clinical preceptor to submit a mid-rotation preceptor evaluation form. This allows the preceptor to communicate with the program how a student is performing and to intervene should improvement be required.
At the end of the clinical rotation, the clinical preceptor will complete an end-of-rotation final preceptor evaluation of the student. The final preceptor evaluation directly correlates to the learning outcomes found in the course syllabus. The final preceptor evaluation comprises 25% of the student’s final grade in the course. For additional information regarding the final preceptor evaluation, please refer to the Preceptor Guide to End-of-Rotation Evaluation document.
- Is there a stipend for being a clinical preceptor?
Yes, we are pleased to offer a stipend for our clinical preceptors who are willing to precept a minimum of three (3) clinical students per clinical year. Clinical preceptors must complete and submit the required documentation to receive the stipend. For more information, contact our program Clinical Coordinator, Esther Castilleja, at esther.castilleja@hsutx.edu
- Can I claim Category I continuing medical education (CME) hours for precepting?
Yes,the HSU PA program has partnered with AAPA to award AAPA Category I CME for PA clinical preceptors. Your AAPA Category I CME is awarded at a rate of 2 CME per PA student per 40-hour week, without limit.
- Is there a title given by the HSU PA program for precepting?
Yes, in recognition of our ongoing appreciation of the service provided to our students, we give titles and recognitions based on the number of students a preceptor takes per cohort. We highly encourage you to add these titles to your curriculum vitae/resume. Preceptors who precept one or two students per cohort are given the title of Clinical Instructor. Preceptors who precept three to four students per cohort are given the title Recognized Clinical Instructor. Preceptors who precept five or more students are given the title Distinguished Clinical Instructor.
Number of Students Precepted Title 1-2 Clinical Instructor 3-4 Recognized Clinical Instructor 5+ Distinguished Clinical Instructor -
Physician Assistant Program Handbooks and Policies
The following policies, in full, can also be found in the HSU PA Student Handbook at the pages listed in the table.
ARC-PA Standard Description of Policy Published Policy and Procedures Page Number A1.02 f Faculty and staff grievances and allegations of harassment DISCRIMINATION / HARASSMENT POLICY
The Hardin-Simmons University PA program has a zero-tolerance policy for discrimination and harassment. Any student, faculty, or staff member is obligated to report incidences witnessed or observed. Whistle blower protection is in place to protect against retaliation. Reports will trigger automatic investigations. Unacceptable conduct includes but is not limited to the following:- Physical harm (e.g., hitting, slapping, kicking) or threats of physical harm
- Requests for performing personal services (e.g., shopping, babysitting)
- Making unwanted sexual advances
- Exchanging sexual favors for grades or other rewards
- Discrimination or harassment based on gender, race/ethnicity, sexual orientation, or religion
- Being subjected to offensive remarks / names based on gender, race/ethnicity, sexual orientation, or religion
- Public embarrassment/humiliation specifically based on gender, race/ethnicity, sexual orientation, or religion
- Denied opportunities for training or awards based on any of the above protected categories (note training opportunities are based upon preceptor availability)
- Receipt of lower grades / evaluations based on protected categories as listed above
For more information refer to the university harassment and Title IX policies which can be found at the HSU website Title IX – Hardin-Simmons University
33 A1.02 g Student allegations of harassment and mistreatment Harassment: In order to promote a safe and comfortable learning environment for all members of the Hardin-Simmons University community, students are expected to conduct themselves in a manner that reflects concern for others in the environment. Examples of behaviors that are unacceptable include but are not limited to theft, vandalism, acts of violence, sexual harassment, and disrespect for personal and University property. If a student has been the recipient of behaviors that may be construed as harassment and is unable or uncomfortable addressing the behavior directly with the involved person(s), the student is encouraged to discuss the situation with their faculty advisor or the Program Director for support and guidance in navigating through Department or University harassment policies and procedures.
Hardin-Simmons University takes the health and safety of our students seriously. If you, or someone you know, believe you have been a victim of sexual misconduct, contact HSU’s Title IX Coordinator at 325-670-1253, office is located on the second floor of the Moody Student Center.
A special note on sexual harassment: Because of the personal nature of patient-provider interactions and the close working relationship of PAs with other members of the healthcare team, it is vital that PAs have a strong working understanding of the behaviors that may be construed as sexual harassment and clearly avoid them. Please see the HSU Sexual Harassment and Misconduct Policy at the following link: HSU-Title-IX-Policy-10-14-22.pdf
For more information, see the HSU Student Handbook which can be found atCurrent Students – Hardin-Simmons University40 A1.02 h Refunds of tuition and fees Tuition, Fees and Other Expenses: The University reserves the right to change tuition and other charges at the beginning of any semester. The tuition cost for a full-time course load does not include expenses for required items such as textbooks, medical equipment and supplies, laboratory fees, and clinical tracking software fees. PA students are not eligible for part-time enrollment unless a specific degree plan is approved as part of a remediation plan after matriculation. In-state and out-of-state tuition are the same.
Deposit: There is a non-refundable $1200.00 deposit, subject to change, for those applicants accepted into the Hardin-Simmons University Physician Assistant Program, which is applied to the tuition for the first semester upon enrollment. If an applicant accepted into the Program encounters circumstances that prevent their matriculation, any amount paid by the applicant to the University that is over and above the non-refundable deposit of $1200.00 will be refunded based on the tuition refund policy set forth by the University and outlined in the University student catalog
Refund Policy – Hardin-Simmons University24-27 A3.02 Student work policy EMPLOYMENT: Because of the rigor of the academic and clinical education phases of the PA Program, outside employment is strongly discouraged. In the event that a student decides to maintain employment during their training, work schedule conflicts will not be acceptable excuses for missing academic activities and clinical rotations will not be scheduled to accommodate a student’s employment.
Students may not be employed by the PA Program. While a student may be invited by a faculty member to volunteer to share their expertise in a specific area with the class, a student may not substitute for or function as instructional faculty and cannot be compelled to share any previous experience with the class. Also, during supervised clinical experiences, students may not substitute for clinical or administrative staff at the clinical site or for the preceptor.34 A3.03 Student teaching policy TEACHING OUT POLICY: In accordance with the SACSCOC requirements, that is, those of the University’s regional accreditor, specific people at Hardin-Simmons University have been charged with responsibility for developing a teach-out plan for currently matriculated students in the event of program closure or loss of accreditation. The Program Director and Dean will work with the University’s SACSCOC liaison to develop a teach-out plan; a written plan to provide for the equitable treatment of students who have not yet completed their program of study. If necessary, to achieve that goal, the teach-out plan may include a teach-out agreement between institutions.
The teach-out plan will be submitted to SACSCOC for approval in advance of implementation. Any teach-out plan will include the following information:- The date of closure (date when new students will no longer be admitted);
- An explanation of how affected parties (students, faculty, staff) will be informed of the impending closure;
- An explanation of how all affected students will be helped to complete their programs of study with minimal disruption;
- An indication as to whether the teach-out plan will incur additional charges/expenses to the students and, if so, how the students will be notified;
- Copies of signed teach-out agreements with other institutions, if any; and
- How faculty and staff will be redeployed or helped to find new employment.
93 A3.04 Clinical student identification IDENTIFICATION: All students will be provided with a university identification badge, including name and photo, clearly identifying each student as a Hardin-Simmons University Physician Assistant (PA) student. Students are required to wear these badges at all times when participating in PA professional functions such as a health fair or when in patient care areas. In clinical practice settings, students must identify themselves as PA students to patients and healthcare practitioners. This badge must be returned to the Program upon graduation or after withdrawal from the Department of Physician Assistant Studies. The first ID badge is free. Replacement badge is $15.00.
Under Student Guidelines:- 1. The student will be clearly identified to distinguish them from physicians, residents, and other health professional students. In the clinical setting, business professional attire, HSU Student ID badge, along with a short white lab coat embroidered with the HSU PA logo is required to always be worn, unless otherwise directed by the site. For example, men should wear a shirt, tie, dress slacks and dress shoes. Women should wear dress blouse and dress slacks. Closed toe shoes must always be worn. Long hair must be pulled up off the neck.
29, 85 A3.05 Student exposure to infectious and environmental hazards INFECTIOUS DISEASE / ENVIRONMENTAL EXPOSURE: The Hardin-Simmons University Department of Physician Assistant Studies has a commitment to protect the health and well-being of students, faculty, staff, and patients. As part of their training, students may encounter exposure to infectious and environmental hazards. This may include, but is not limited to, being exposed to human cadavers and preservative chemicals such as formalin in the anatomy lab, latex or other products such as gloves that may contain allergens, and exposure to communicable infectious disease which may be transferred in the classroom or clinical setting. PREVENTION: While the risk of transmission is small, the Program has policies and procedures in place to minimize risk.
It is the policy of the Hardin-Simmons University, Physician Assistant Program to follow the guidelines and recommendations made by the Centers for Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration (OSHA) regarding standard precautions. Before beginning clinical education experiences through the HSU Physician Assistant Program, students will receive training regarding CDC standard precautions as well as OSHA training.
Standard Precautions
Standard Precautions combine the major features of Universal Precautions and Body Substance Isolation and are based on the principle that all blood, body fluids, secretions, respiratory particles, excretions, non-intact skin, and mucous membranes may contain transmissible infectious agents.
Standard Precautions include a group of infection prevention practices that apply to all patients, regardless of suspected or confirmed infection status, in any setting in which healthcare is delivered. These practices include:- Hand hygiene
- The use of personal protective equipment (PPE)
In addition to Standard Precautions, students will receive training in the three categories of Transmission-Based Precautions:- Contact Precautions
- Droplet Precautions
- Airborne Precautions
Transmission-Based Precautions are used when the route(s) of transmission is (are) not completely interrupted using Standard Precautions alone.
Students may access details of this information at any time at the following website:
Isolation Precautions Guideline | Infection Control | CDC79-80 A3.06 Provision of healthcare POLICY REGARDING FACULTY HEALTHCARE: PA Program Principal Faculty, Instructional Faculty, Program Director, and Medical Director will not participate as healthcare providers for students in the Program. It is acceptable for healthcare to be provided in an emergency only until licensed emergency personnel arrives. 30 A3.07 Referral to student services Mental Health/Counseling: The Office of Student Life offers free counseling services to students. A provider referral is not necessary. Students may contact counseling services directly through email or calling. Counseling service will respond to inquiries within 1-2 business days. Additional information about these services can be found at the following website:Counseling Services – Hardin-Simmons University
Suicide hotlines are available 24 hours a day to students and links are made through these services to local providers on campus for interventions when needed. The National Suicide Prevention Hotline phone number is (800) 273-TALK (8255).30 A3.08 Clinical site / preceptor recruitment PRECEPTOR SOLICITATION POLICY: Students are not required to provide or solicit their own clinical sites or preceptors for their supervised clinical practice experiences (SCPEs). The Hardin-Simmons University PA Program’s Director of Clinical Education and the clinical team are responsible for coordinating, recruiting, providing, and securing all program-required SCPEs.
Students are welcome to provide contact information for potential clinical sites or preceptors to the clinical team. However, please note that submitting a suggestion does not guarantee the site will be recruited or that the student will be placed there. All potential sites must first be vetted and approved by the program to ensure they meet program requirements.89 A3.09 Immunization & health screening HEALTH, IMMUNIZATIONS AND HEALTH INSURANCE:
As part of the matriculation process into the PA Program, the Department of Physician Assistant Studies requires all students to meet the health and immunization requirements listed in Appendix B of this document. If a student chooses not to be vaccinated or tested, they will forfeit their seat in the program. Immunizations will not be required if the student has a specific medical contraindication to the required vaccine(s). Students must provide documentation from their healthcare provider of any adverse reaction or contraindication to a required vaccine(s).
Hardin-Simmons University PA Program immunization policy is aligned with the Centers for Disease Control and Prevention (CDC) Immunization of Health-Care Personnel: Recommendations of the Advisory Committee on Immunization Practices (ACIP).
Prior to matriculation in the Program, all students must complete the Hardin-Simmons University PA Program Immunization Verification Document and Health Clearance Form, have a physical examination by a healthcare provider, and have their healthcare provider complete the attestation form of fitness to proceed in the PA Program (located at the end of this handbook, Appendix B & C). Official documents must be completed by a medical provider that is not related to you. Additionally, proof of personal health insurance must be provided prior to matriculation and maintained throughout the Program.
The Hardin-Simmons PA program’s clinical sites all require the immunizations and screenings listed on the Immunization Verification Document. Some immunizations and screenings may need to be repeated on an annual basis due to clinical site requirements. Unless there is a documented medical contraindication, all students must have these vaccines in order to complete the program. Immunizations will not be required if the student has a specific medical contraindication to the vaccines listed. Students must provide documentation of any adverse reaction or contraindication to a vaccine required. In addition, a licensed medical provider should certify the contraindication. Again, the form cannot be completed or signed by a family member who is in the medical field.
Various clinical training sites may require additional immunizations, evidence of testing, or titers prior to rotations, to include COVID-19. Fulfillment of these requirements, and any associated costs, will be the student’s responsibility. If students choose not to be vaccinated or tested, they will not be allowed to rotate at clinical sites that require the additional immunization(s) and/or testing. Inability to rotate at clinical sites due to noncompliance with required immunizations/testing is not the responsibility of the program. If the student is voluntarily non-compliant with rotation site policies for screening/immunizations on all rotations, graduation will be delayed, or the student may be ineligible for graduation from the PA Program. Immunizations will not be required if the student has a specific medical contraindication to the vaccines listed. Students must provide documentation from a healthcare provider of any adverse reaction or contraindication to a vaccine required.
PA student health records are confidential and will not be accessible to, or reviewed by, Program, Principal Faculty, instructional faculty, Medical Director, or staff except for immunization and tuberculosis screening results which may be maintained and released with written permission from the student.
Recommendations may vary for pregnant women and those with health conditions or allergies. Please refer to your healthcare provider or CDC website for updates and clarifications regarding specific immunization requirements.
Please contact your healthcare provider and/or refer to CDC websites below for updates and clarifications regarding specific immunization requirements: Recommended Vaccinations for Adults | Vaccines & Immunizations | CDC
International Mission Immunization Requirements:
In addition to the above health and immunization requirements for all HSU PA students, there will be supplementary immunization and health requirements for students going to international missions. These immunizations will be at the student’s expense. This will include any routine and required immunizations and health recommendations for the country as recommended by the Centers for Disease Control and Prevention Travel Medicine website at: Destinations | Travelers’ Health | CDC.
Students traveling abroad will also be instructed to follow safety precautions for the country of interest which are available through the US Department of State website: Travel.30-31 A3.11 Program Competencies HSU PA PROGRAM COMPETENCIES:
Upon completion of the program, students are expected to demonstrate competency in the following domains:- Medical knowledge,
- Clinical reasoning and problem-solving abilities,
- Clinical and technical skills,
- Interpersonal skills, and
- Professionalism.
- Apply foundational medical sciences to inform clinical decision-making and management of patients. (medical knowledge; clinical reasoning & problem solving)
- Accurately obtain and document a medical history, including chief complaint, medical, family, social history, and review of systems, to support clinical decision-making. (clinical and technical skills)
- Demonstrate proficiency in performing a physical examination, utilizing appropriate techniques to assess body systems based on the patient’s clinical presentation and history. (clinical and technical skills)
- Assess and apply knowledge of disease etiology, epidemiology, and risk factors to identify health conditions in both symptomatic and asymptomatic individuals. (medical knowledge, clinical reasoning & problem solving)
- Demonstrate the ability to apply risk-appropriate patient screenings using evidence-based guidelines to identify health risks, promote disease prevention, and support early disease detection across the life span. (medical knowledge, clinical reasoning & problem solving)
- Demonstrate the ability to recognize, assess, and address social determinants of health that impact patient outcomes and healthcare delivery, applying this understanding to promote equitable, patient-centered care across diverse populations. (medical knowledge, clinical reasoning & problem solving, professionalism)
- Apply evidence-based clinical reasoning and problem-solving skills to demonstrate comprehensive, systems-based knowledge across the spectrum of clinical medicine. (clinical reasoning & problem solving)
- Competently perform clinical and technical skills essential for the evaluation and management of patients. (clinical & technical skills)
- Accurately order and interpret diagnostic and laboratory data to support clinical decision-making. (medical knowledge, clinical reasoning & problem solving)
- Synthesize acquired patient history, physical examination findings, and diagnostic data to formulate a differential diagnosis and a comprehensive assessment, incorporating evidence-based practices. (medical knowledge; clinical reasoning & problem solving)
- Formulate and implement patient-centered treatment plans and interventions based on clinical assessment, evidence-based guidelines, and individual patient needs across the life span. (clinical reasoning & problem solving)
- Demonstrate responsible prescribing practices by applying knowledge of pharmacologic agents, including their indications, contraindications, side effects, interactions, and potential adverse reactions, to ensure safe and effective patient care. (medical knowledge, professionalism)
- Communicate test results, treatment plans, and health-related information to patients in a clear, culturally sensitive, and confidential manner to support informed decision-making and patient-centered care. (interpersonal skills, professionalism)
- Communicate patient information effectively with members of the healthcare team through clear oral presentations and accurate, concise written documentation. (interpersonal skills, clinical & technical skills)
- Exhibit professionalism, respect, and ethical behavior in both educational and clinical environments. (professionalism)
- Demonstrate a foundational knowledge of the physician assistant profession, the roles and responsibilities of various health professionals, and the principles of interprofessional collaboration essential to effective team-based healthcare. (medical knowledge)
- Demonstrate the ability to critically appraise, conduct, and disseminate scholarly research that contributes to the advancement of clinical knowledge and practice, aligning with the principles of evidence-based medicine. (medical knowledge, clinical reasoning & problem-solving)
11-12 A3.14 a Academic standards ACADEMIC POLICIES/STANDARDS:
General Academic Requirements- Grade Point Average (GPA): Students must maintain a cumulative 3.0 GPA or higher in all graduate coursework. When a course is repeated, only the most recent grade will be used to calculate the GPA.
- Grading Standards: Students may not obtain a grade of ‘D’ or ‘F’ in any graduate course.
- A student will be placed on academic probation if their cumulative GPA falls below 3.0 or if they receive a grade of ‘D’ or ‘F’ in any graduate course provided they are allowed to remain in the program.
- A student on academic probation is not eligible to graduate.
- To return to good academic standing, a student must meet the requirements set by their graduate advisory committee and achieve a cumulative GPA of 3.0 or better.
In addition to the general academic requirements, students in the didactic curriculum must meet these specific standards:- Course Grades: Students must earn a final course grade of ‘B’ (80%) or higher in all didactic courses.
- Probation: A student who earns a course grade of ‘C’ in a didactic course will be placed on academic probation.
During the clinical curriculum, students may earn a final course grade of ‘C’ (70-79%), provided they maintain the minimum 3.0 GPA requirement.
Grading System:
The Physician Assistant Program uses the following grading scale. The final course/rotation grade will be recorded as “A”, “B”, “C”, or “F”.- A = 90%–100%
- B = 80%–89%
- C = 70%–79%
- F = <70%
Rounding up of grades is only done at the end of a course, not for individual tests or assignments, and only if greater than 0.50.
50 A3.14 b Program completion GRADUATION REQUIREMENTS:
A student’s readiness to advance from the didactic to the clinical phase and to graduate from the PA program is determined by several key performance indicators. These include: successfully completing all courses, achieving the required grade point average, demonstrating proficiency in clinical and technical skills, exhibiting consistent professionalism, fulfilling volunteer hour requirements, passing all summative examinations, and completion of all requirements for the Capstone Research Project.
Students who have been recommended for graduation by the HSU PA Program Grading and Promotions Committee will be awarded the Master of Physician Assistant Studies (MPAS) degree provided they have met all of the following conditions and adhere to the policies outlined in the PA student handbook and the Hardin-Simmons University Graduate handbook.
Requirements for Graduation- Satisfactory completion of 21 courses during the didactic phase of the curriculum earning 53 credit hours and achieving a minimum overall 3.0 grade point average (GPA).
- Satisfactory completion of all 10 clinical rotations and three additional post-clinical courses for a total of 13 courses, earning 59 credit hours, and achieving a minimum overall 3.0 grade point average (GPA).
- Completion of three formative Objective Structured Clinical Examinations (OSCEs) during the clinical phase of the curriculum.
- Documentation of competency of all required technical skills within the didactic and clinical phases of training as denoted by instructional or principal faculty.
- Satisfactory completion of all course requirements for the Capstone Research project.
- Satisfactory demonstration of the ethical, professional, behavioral, and personal characteristics as documented on the professionalism evaluation forms listed below:
- End-of-semester professional evaluation forms during the didactic year,
- Preceptor evaluation forms during the clinical year, and
- The final summative professional assessment by the Program Director within 4 months of graduating.
- Satisfactory completion of all summative assessment components administered within 4 months before graduation from the program with a grade of 70% or greater:
- Summative OSCE,
- End of curriculum written exam, and
- Clinical & technical skills assessment
- Completion of a minimum of 50 hours of community service hours of which 20 hours must be completed by the end of the didactic year.
- Completion of a diploma card with the Hardin-Simmons University Registrar’s office.
- Satisfactory payment of all fees due to the University and meets all requirements for commencement per university policy.
- Completed any terms of Academic Probation and/or Remediation if applicable.
Students unable to fulfill these requirements by the day of graduation will not be allowed to participate in the commencement ceremony without the permission of the PA Program Director. Students will not be considered graduates in any capacity until they have completed all of the above requirements.
91 A3.14 c Remediation policies REMEDIATION:
The Hardin-Simmons University PA Program monitors and documents the progress of each student in a manner that promptly identifies deficiencies in knowledge or skills and establishes means for remediation.
Academic advisors are assigned to each student at new student orientation and remain with the student throughout the Program. These advisors meet with students at minimum once each semester and are notified of any academic performance or professionalism concerns noted by instructors, preceptors, and faculty throughout the course of the Program. Performance <70% on any one assessment will require a meeting with the student advisor for academic counseling and implementing a strategy for success in the future. Problem areas can be identified in these meetings and addressed as appropriate. Students may also be referred for counseling through the student resources on campus if personal issues are interfering with their academic performance. The academic advisor will globally review the student’s areas of strength and weakness at the end of each semester and provide feedback and action plans as needed on a case-by-case basis.
Students are assessed on academic content through formative and summative evaluations. The goal of formative assessment is to monitor a student’s learning and provide feedback to the student to improve their understanding of the material. Formative assessments identify a student’s strengths and weaknesses and target areas that need improvement. Additionally, formative assessment allows faculty to identify students who are struggling and who may benefit from remediation. Formative assessments are generally low stakes and examples include, but are not limited to: quizzes, concept mapping, assignments, and summary papers.
Summative assessments evaluate a student’s learning at the end of an instructional unit/module and/or course. Summative assessments are high stakes, and examples include, but are not limited to: end-of-module examinations, comprehensive final examinations, a final research project, and a research paper.
During the didactic year, if a student scores less than 80% on a formative assessment, the student is encouraged to contact the course instructor for content clarification and remediation to include identification of areas of strengths and weaknesses.
If a student scores less than 80% on a summative assessment, the student is required to meet with the course instructor for content remediation. The student should contact the course coordinator within 48 hours of receiving notification of a failed summative examination to schedule a meeting. Content remediation should be in the form of additional formative assignments to reevaluate the student’s understanding of the material. After remediation, reassessment is required to ensure the student has been remediated to competency. Reassessment methods may include retesting through a multiple-choice examination, a comprehensive final, an oral examination, or a proctored written assessment. The score earned on the reassessment must be greater than or equal to 80% to demonstrate competency. The reassessment score will not replace the original score.
If a student scores less than 80% on the final comprehensive examination, the student is required to meet with the course instructor for content remediation. The student should contact the course coordinator within 48 hours of receiving notification of the failed comprehensive final examination. The student will be given an incomplete (I) for the final grade recorded in the class until the student has undergone remediation and reassessment outlined in the didactic policies below. See Phase II-A below.
Students requiring formal academic remediation will be identified by the faculty through progress monitoring of content areas as well as by those that do not maintain scores of 80% or higher on coursework. Globally at-risk students will be identified at the end of each semester by analysis of performance compared to peers.
Additional detailed remediation policies for the didactic curriculum can be found on pages: 52-64
Additional detailed remediation policies for the clinical curriculum can be found on pages: 64-69
51 A3.14 d Deceleration policies DECELERATION POLICY:
Deceleration is an alternative mechanism that allows students to complete the Hardin-Simmons University Physician Assistant program curriculum. Deceleration may allow students to extend their curriculum due to academic deficiencies. Reasons for deceleration can be either voluntary or mandatory.
Voluntary Deceleration: Students must submit a written request to the Program Director to voluntarily decelerate by taking a leave of absence. Voluntary deceleration is considered a proactive decision on the part of the student before experiencing academic difficulty. If voluntary deceleration occurs during the didactic training, the student will reseat in August with the incoming class and must meet all previously agreed upon conditions as outlined in the Leave of Absence Policy.
Mandatory Deceleration: The Grading and Promotions Committee may recommend deceleration to the Program Director to remediate deficiencies, as a preventative measure to avoid further academic difficulty, or as a result of non-academic reasons as defined in the student handbook. The Committee may specify the plan for deceleration or defer to the judgment of the Program Director. Students in the decelerated curriculum must successfully complete all required courses. Upon decelerating, students may delay their graduation by no more than one year and must comply with any revisions in curriculum requirements and changes in tuition and fees of their new graduating class. A unique degree plan will be created for any decelerated student. The student will be required to audit and/or repeat courses previously passed and repeat any course(s) in which a grade of C was obtained. If the student fails any course(s) the student will be dismissed from the Program immediately. If a student earned less than a C in any course, they are not eligible to reapply.
A maximum of 4 years will be allowed to complete all aspects of the program from first matriculation date.73 A3.14 e Withdraw policies WITHDRAWAL: A student who finds it necessary to withdraw from the University before the end of the semester must secure the proper form for withdrawal through the Office of the Registrar. The form requires approval by the Business and Financial Aid Offices. If procedure is not followed, the student is automatically assigned a grade of “F” in all courses. However, no student may withdraw after the last date of withdrawal specified in the academic calendar. See leave of absence and deceleration policies for information regarding returning to the PA Program.
At no time will the Program Director or Faculty be aware of a student’s medical condition. The documentation that validates the legitimacy of the student’s case will be contained in the Office of the Dean of Students in the area of Student Life and Counseling.73 A3.14 f Dismissal policies DISMISSAL POLICY:
The HSU PA Program, in alignment with university standards and the rigorous demands of the medical profession, has established clear and transparent policies regarding student progression and, when necessary, dismissal from the program. Student progress is consistently monitored by the Grading and Promotions Committee to ensure that all students meet the academic and professional standards required for entry into clinical practice.
Grounds for Dismissal
A student may be subject to dismissal from the HSU PA Program for failure to comply with the established academic and/or professional standards. Dismissal may occur at any time during the didactic or clinical phases of the curriculum.
1. Academic Dismissal
A student may be dismissed from the program for any of the following academic reasons:
- Failure to meet the terms of academic probation: The Grading and Promotions Committee will place a student on academic probation if their academic performance falls below program standards. Failure to meet the specific requirements of this probationary period may result in dismissal.
- Failure to meet published academic standards while on academic probation: Students on academic probation must adhere to all published academic standards. Any further academic issues while on probation may lead to dismissal.
- Failure to meet the published academic improvement contract: If a student is required to complete an Academic Improvement Contract, failure to successfully fulfill its terms may result in dismissal.
- Final grade deficiencies in the didactic curriculum:
- Earning a final grade of a “C” in two or more didactic courses during the same semester.
- Earning a final grade of “C” while on academic probation
- Earning a final grade below a “C” in any didactic course.
- Cumulative GPA requirement: Failure to maintain or raise the cumulative 3.0 GPA required by the university.
- Clinical year examination failure: Failure of a third End of Rotation (EOR) examination during the clinical year.
- EOR failure while on academic probation: Failing an EOR exam while a student is on academic probation will result in dismissal.
- Final grade deficiencies in the clinical curriculum:
- Earning a final grade below a “C” while on academic probation
- Earning a final grade below a “C” in a second clinical course
- Failure to pass summative evaluation: Failure to pass the reassessment of any portion of the summative evaluation may result in dismissal.
2. Professional Dismissal
A student may be dismissed from the program for any of the following professional reasons, as determined by the Grading and Promotions Committee:
- Egregious violations of the Standards of Professional Conduct: This includes, but is not limited to, actions that pose a risk to patient safety, demonstrate a lack of professional judgment, or severely violate ethical principles.
- Repeated violations of the Standards of Professional Conduct: A pattern of unprofessional behavior, even if individual incidents are minor, can lead to dismissal.
- Violation of the Academic Integrity Policy: Any violation of the university’s academic integrity policy, including cheating or plagiarism, may result in immediate dismissal.
- Preceptor evaluation failure: A second failure of a preceptor evaluation during the clinical year.
- Intoxication or use of illegal substances: Being under the influence of alcohol or illegal substances during any program activity, including class, lab sessions, or clinical rotations, is strictly prohibited and will result in dismissal.
- Misrepresentation: Misrepresenting themselves as a licensed medical provider, either verbally or in writing, is a direct violation of professional standards and will lead to dismissal.
- Failure to meet technical standards: Failure to meet the program’s published technical standards, even with reasonable accommodations, may result in dismissal.
71-72 A3.14 g & h Student grievances and appeals GRADE APPEAL PROCESS / GRIEVANCE:
Academic Grievance Policy
The following measures should be taken with respect to an academic grievance pertaining to a course offered by the University. A student may seek remediation for the following:
a. Grade Appeal: A student who feels that the grading policy for a class is unfair or has been unfairly administered and that the result is a course grade lower than deserved has the right to contest the professor’s decision. This process is only for appealing the final course average; consequently, grades on individual projects may not be challenged.
b. Course-Related Concern: Any complaint, beyond the parameters of a grade appeal, which involves an experience occurring within the context of an academic course offered by the University also comes under the purview of the Academic Grievance Policy.
Arbitration for either (a) Grade Appeal or (b) a Course-Related Concern follows the same procedure, with exceptions noted below.
Informal Measures
The University encourages matters to be resolved informally and judiciously whenever possible. If such an agreement is unable to be reached, then a student may file a formal complaint. Each step must be taken in order. Failure to follow the procedure may obviate the appeal.
Step 1. The student discusses the matter with the professor. If possible, the matter is reconciled at this point.
Step 2. If dissatisfied with this discussion, the student voices concern to the department head in a conference scheduled by the student. (If no department head exists, or if the department head is a disputant, then the student consults with the dean of the college or school in which the course under consideration is offered.) The department head (or, if applicable, the dean) discusses the matter with the professor.
Step 1 and Step 2 attempt to find an amicable resolution to the academic grievance informally—be it either (a) Grade Appeal or (b) a Course-Related Concern—without a formal, written complaint. If no resolution occurs in the first two steps, then formal measures may be taken beginning with Step 3.
Formal Measures
Step 3. If no resolution occurs at the department level (Step 2), the student then submits a written petition to the dean of the area. If the complaint is against a dean, the complaint will go to the provost. The student’s letter of petition must include a straightforward narrative (one to three pages in length) detailing (a) the circumstances surrounding the contested grade or course-related concern, (b) reasons why the student believes the complaint is warranted, and (c) what possible outcome or resolution, from the student’s perspective, will resolve the issue at hand.
If the grievance is a grade appeal, then all graded projects in the class—tests, essays, projects, etc.— that are in the student’s possession must be submitted along with the cover letter along with the student’s personal record of attendance in the class.
Upon the dean’s notification that a student has filed a formal grievance, the department head forwards a written summation of the matter to the dean, along with a recommendation for a resolution to the problem. (If no department head exists, or if the department head is a disputant, then a letter from the department head is not necessary.)
Step 4. In writing, the dean apprises the professor of the course under dispute regarding the student’s grievance and provides a summary of the points of concern.
Step 5. The professor submits a written response to the student’s grievance in a straightforward narrative (one to three pages in length) detailing his or her own account of (a) the circumstances surrounding the contested grade or course-related concern, (b) reasons why the professor believes the complaint either warranted or unwarranted, and (c) what possible outcome or resolution, from the professor’s perspective, will resolve the issue at hand. If the grievance is a grade appeal, then the professor appends the student’s projects in the professor’s possession, grades on all work done in the course, the student’s attendance record in the class, and a copy of the class syllabus with the contested policy clearly marked.
Step 6. The dean will meet with each party separately, or jointly, to seek a viable solution.
Step 7. If no solution can be reached with Step 6, then (a) a formal Grade Appeal goes to arbitration before the Academic Grievance Committee. The dean submits all materials involved up to this point, along with a written recommendation for a solution to the problem to the committee.
Membership of the Academic Grievance Committee:
The committee includes three professors from different academic areas with one specified to the chair and two senior students with grade point averages of at least 3.0. The chair of the committee will schedule meetings and preside over deliberations. Neither the professor nor the student will have counsel at the meetings.
Duties of the Academic Grievance Committee:
The committee will review materials submitted by both student and professor before coming together in session and convene at a time convenient for all involved for the purpose of hearing both parties present their cases. Committee members will then hold an executive session to reach a decision. The chair of the committee will inform the student, the faculty member, and the provost of their decision in writing. If a grade is to be changed, the provost will see that the proper forms are submitted to the Office of the Registrar. The ruling of this committee is final with respect to grade appeals.
A formal Course-Related Concern goes directly to the Provost and Chief Academic Officer for resolution. The dean submits all materials involved up to this point, along with a written recommendation for a solution to the problem to the Provost, who will then review materials submitted by both student and professor before scheduling a time, convenient for all involved, for the purpose of hearing both parties present their cases. The provost, at his or her own discretion, may seek additional counsel as appropriate.
The ruling of the provost is final.
Refer to the HSU Student Handbook at: HSU PA Student Handbook76-77 A3.14 i Student employment EMPLOYMENT: Because of the rigor of the academic and clinical education phases of the PA Program, outside employment is strongly discouraged. In the event that a student decides to maintain employment during their training, work schedule conflicts will not be acceptable excuses for missing academic activities and clinical rotations will not be scheduled to accommodate a student’s employment.
Students may not be employed by the PA Program. While a student may be invited by a faculty member to volunteer to share their expertise in a specific area with the class, a student may not substitute for or function as instructional faculty and cannot be compelled to share any previous experience with the class. Also, during supervised clinical experiences, students may not substitute for clinical or administrative staff at the clinical site or for the preceptor.34 A3.14 j SCPE Travel Policy TRAVEL TO CLINICAL SITES: The HSU PA Program offers students a wide variety of supervised clinical practice experiences (SCPEs) in diverse settings, including hospitals, clinics, private offices, and emergency departments. These rotations are located in the Abilene area, across the state of Texas, as well as out-of-state locations.
Students should be prepared for rotations that may require travel. Students may be assigned up to two (2) SCPEs more than 500 miles away from the program. Students will be required to complete up to three (3) rotations more than 200 miles (but less than 500 miles) away from the program. All students are required to complete at least one SCPE in a rural or underserved setting.
Students are responsible for all travel and housing expenses related to their SCPEs, including any airfare if they choose to fly. The clinical team works to reduce this financial burden by using student input on housing availability when making clinical rotation assignments. Data is collected annually from current clinical students to provide estimates of additional travel and housing expenses and this information is included in the estimated cost of attendance.89 -
Tuition and Fees for the Physician Assistant Studies Program
Total Cost of the Program
The PA Program makes every effort to keep costs reasonable for students. However, because the Program runs continuously for twenty-seven months, applicants must review their financial resources carefully and anticipate expenses realistically. During the clinical education phase, all students may be assigned to clinical sites outside of the immediate Abilene / Big Country area. The student is responsible for the costs related to out-of-area travel and housing, if applicable.
The total tuition and fee cost of the Program is estimated at $107,912 – $116,117, depending on year of entry into the Program. Updated accurate tuition and fee costs are published on the university web site at www.hsutx.edu/pa. This does not include living expenses, textbook or equipment costs. The estimates for these costs vary based on student choice of housing, family size, transportation/vehicle cost, and technology related costs (laptop computer, data plan, and mobile phone required). Reliable transportation is required in the clinical year for commuting to supervised clinical practice experiences (SCPE).
Learn more about what makes up cost of attendance and how to request a cost of attendance adjustment when additional education-related expenses beyond a student’s standard COA are incurred.
Program Tuition & Fees
COHORT STARTING: 2023 Fall – Graduating 2025 Tuition: $97,900 (entire program) + $9,100 (Estimated University Fees) Breakdown of University Fees: Departmental Examination Fee (per semester) $40/Semester $280.00 Departmental Laboratory Fee (per semester) $80/Semester $560.00 General Student Fee (will vary per semester) Estimate of fee is $520.00/Semester $3,640.00 Student Insurance Fee $40/year (3 years) $120.00 Clinical Placement fee ($500/clinical course x 9 courses) $4,500.00 Total University Fees are approximately $9,100.00 Breakdown of Non-University Fees: EXXAT Fees: ~$369.00 – one-time fee $369.00 Medical Terminology: ~$140.00 – one-time fee $140.00 American Academy of Physician Associates: $75.00 – one-time fee $75.00 Texas Academy of Physician Assistants: $25.00 – one-time fee $25.00 Background Checks: $72.00 + tax (for TX and NM residents) each – a minimum of 3 background checks per student $216.00 Drug Screens $29.00 + tax (for TX and NM residents) each – a minimum of 3 drug screens per student $87.00 *Non-University Fees are approximately $912.00 *All fees are subject to change
Total Estimated Tuition & Fees for Graduating 2025: $107,912.00 All tuition and fees are the same for Resident & Non-Resident students.
“Semester” for the PA Program means three (3) per year: Spring, Summer, and Fall for a total of seven (7) semesters for the entire program.
Cost of books, equipment, and living expenses will vary based on individual student lifestyle choices. Electronic book options, purchase of used books, and/or rental of textbooks may offset costs.
Estimated Textbook Expenses $2,900 Estimated Equipment Expenses $1,000 Estimated additional monthly expense for travel and housing for SCPEs* during clinical year ($1500 x 9 SCPEs) $13,500 *SCPE = supervised clinical practice experiences Total Estimated Cost of Program $125,312 COHORT STARTING: 2024 Fall – Graduating 2026 Tuition: $102,800 (entire program) + $9,100 (Estimated University Fees) Breakdown of University Fees: Departmental Examination Fee (per semester) $40/semester $280.00 Departmental Laboratory Fee (per semester) $80/semester $560.00 General Student Fee (will vary per semester) Estimate of fee is $520.00/semester $3,640.00 Student Insurance Fee $40/year (3 years) $120.00 Clinical Placement fee ($500/clinical course x 9 courses) $4500.00 Total University Fees are approximately $9,100.00 Breakdown of Non-University Fees: EXXAT Fees: ~$369.00 – one-time fee $369.00 Medical Terminology: ~$140.00 – one-time fee $140.00 American Academy of Physician Associates: $75.00 – one-time fee $75.00 Texas Academy of Physician Assistants: $25.00 – one-time fee $25.00 Fingerprinting $35.00 Background Checks: $72.00 + tax (for TX and NM residents) each – a minimum of 3 background checks per student $216.00 Drug Screens $29.00 + tax (for TX and NM residents) each – a minimum of 3 drug screens per student $87.00 *Non-University Fees are approximately $947.00 *All fees are subject to change
Total Estimated Tuition & Fees for Graduating 2026: $112,847 All tuition and fees are the same for Resident & Non-Resident students.
“Semester” for the PA Program means three (3) per year: Spring, Summer, Fall for a total of seven (7) semesters for the entire program.
Cost of books, equipment, and living expenses will vary based on individual student lifestyle choices. Electronic book options, purchase of used books, and/or rental of textbooks may offset costs.
Estimated Textbook Expenses $2,900 Estimated Equipment Expenses $1,000 Estimated additional monthly expense for travel and housing for SCPEs* during clinical year ($1500 x 9 SCPEs) $13,500 *SCPE = supervised clinical practice experiences Total Estimated Cost of Program $130,247 COHORT STARTING: 2025 Fall – Graduating 2027 Tuition: $104,900 (entire program) + $9,170 (Estimated University Fees) Breakdown of University Fees: Departmental Examination Fee (per semester) $40/semester $280.00 Departmental Laboratory Fee (per semester) $80/semester $560.00 General Student Fee (will vary per semester) Estimate of fee is $530.00/semester $3,710.00 Student Insurance Fee $40/year (3 years) $120.00 Clinical Placement fee ($500/clinical course x 9 courses) $4,500.00 Total University Fees are approximately $9,170.00 Breakdown of Non-University Fees: EXXAT Fees: ~$369.00 – one-time fee $369.00 Medical Terminology: ~$140.00 – one-time fee $140.00 American Academy of Physician Associates: $75.00 – one-time fee $75.00 Texas Academy of Physician Assistants: $25.00 – one-time fee $25.00 Fingerprinting $35.00 Background Checks: $72.00 + tax (for TX and NM residents) each – a minimum of 3 background checks per student $216.00 Drug Screens $29.00 + tax (for TX and NM residents) each – a minimum of 3 drug screens per student $87.00 *Non-University Fees are approximately $947.00 *All fees are subject to change
Total Estimated Tuition & Fees for Graduating 2027: $115,017 All tuition and fees are the same for Resident & Non-Resident students.
“Semester” for the PA Program means three (3) per year: Spring, Summer, Fall for a total of seven (7) semesters for the entire program.
Cost of books, equipment, and living expenses will vary based on individual student lifestyle choices. Electronic book options, purchase of used books, and/or rental of textbooks may offset costs.
Estimated Textbook Expenses $2,900 Estimated Equipment Expenses $1000 Estimated additional monthly expense for travel and housing for SCPEs* during clinical year ($1500 x 9 SCPEs) $13,500 *SCPE = supervised clinical practice experiences Total Estimated Cost of Program $132,417 COHORT STARTING: 2026 Fall – Graduating 2028 Tuition: $106,000 (entire program) + $9,170 (Estimated University Fees) Breakdown of University Fees: Departmental Examination Fee (per semester) $40/semester $280.00 Departmental Laboratory Fee (per semester) $80/semester $560.00 General Student Fee (will vary per semester) Estimate of fee is $530.00/semester $3,710.00 Student Insurance Fee $40/year (3 years) $120.00 Clinical Placement fee ($500/clinical course x 9 courses) $4500.00 Total University Fees are approximately $9,170.00 Breakdown of Non-University Fees: EXXAT Fees: ~$369.00 – one-time fee $369.00 Medical Terminology: ~$140.00 – one-time fee $140.00 American Academy of Physician Associates: $75.00 – one-time fee $75.00 Texas Academy of Physician Assistants: $25.00 – one-time fee $25.00 Fingerprinting $35.00 Background Checks: $72.00 + tax (for TX and NM residents) each – a minimum of 3 background checks per student $216.00 Drug Screens $29.00 + tax (for TX and NM residents) each – a minimum of 3 drug screens per student $87.00 *Non-University Fees are approximately $947.00 *All fees are subject to change
Total Estimated Tuition & Fees for Graduating 2028: $116,117 All tuition and fees are the same for Resident & Non-Resident students.
“Semester” for the PA Program means three (3) per year: Spring, Summer, Fall for a total of seven (7) semesters for the entire program.
Cost of books, equipment, and living expenses will vary based on individual student lifestyle choices. Electronic book options, purchase of used books, and/or rental of textbooks may offset costs.
Estimated Textbook Expenses $2,900 Estimated Equipment Expenses $1,000 Estimated additional monthly expense for travel and housing for SCPEs* during clinical year ($1500 x 9 SCPEs) $13,500 *SCPE = supervised clinical practice experiences Total Estimated Cost of Program $133,517 -
PA Program Faculty & Staff
Faculty
Tina Butler DMSc, MPAS, PA-C
Program Director, Associate Professor
Dr. Tina Butler is the Program Director for the Hardin-Simmons University Physician Assistant Program. She has been involved in PA education for over 15 years. She previously served as the program’s Associate Program Director and Academic Director. Dr. Butler graduated from the University of Texas Southwestern Medical Center Dallas Physician Assistant Program in 1998, and obtained her Master’s degree in Physician Assistant Studies with an emphasis in Cardiology from the University of Nebraska in 2007. She earned her Doctor of Medical Science in 2020 from the Rocky Mountain University of Health Professions. Dr. Butler has practiced clinically as a PA for over 25 years with the majority of her clinical experience in cardiology. She also has clinical experience in family practice and urgent care settings. Dr. Butler has served on multiple committees at both the state and national level. She served on the Board of Directors for the Texas Academy of PAs (TAPA) for over 10 years and is a Past President of TAPA. Dr. Butler is a published author in both educational and professional journals and has presented at CME conferences and education forums. Currently Dr. Butler chairs the Physician Assistant Education Association (PAEA) Rotation Exam Review Internal/Family Medicine committee. For relaxation, Dr. Butler enjoys reading, spending time with her family, and raising their Great Danes.
Clay Bulls MPAS, PA-C
Assistant Professor
Clay Bulls, of Abilene, is a Physician Assistant who specializes in Hospital Medicine. He works with TeamHealth as a PA in Internal Medicine at Hendrick Medical Center. He is a member of the Texas Academy of Physician Assistants and the American Academy of Physician Assistants. He holds a Certificate of Added Qualifications (CAQ) in Hospital Medicine from the NCCPA. He received his bachelor’s degree from McMurry University and is a graduate of the Wake Forest University School of Medicine Physician Assistant program. He completed his Master of Physician Assistant Studies Degree from the University of Texas Rio Grande Valley. He currently serves as a member of the Texas Physician Assistant Board after being appointed in 2015 by Governor Greg Abbott where he chairs the Discipline and Ethics Committee. Mr. Bulls is an Assistant Professor for the Hardin-Simmons University Physician Assistant Program.
Jessica Lindemood, OBGYN
Assistant Professor
Jessica Lindemood is an Assistant Instructor for the Hardin-Simmons Physician Assistant Program serving in both the didactic and clinical aspects of the program. Her practice background includes Family and Internal Medicine, but she has found her calling in Women’s Health and obtained a certification as a Nationally Certified Menopause Practitioner in 2022. She has been heavily involved in PA education since her graduation from the Texas Tech University Physician Assistant Program in 2010. She has served as a clinical preceptor, guest lecturer, and adjunct instructor as well as having had experience as a former faculty member with the Texas Tech University Physician Assistant Program. In her spare time, she enjoys finding avenues to become actively involved in her community and spending as much quality time as she is able with her with her husband and two young daughters.
Brianna Martinez, MPAS, PA-C
Academic Director, Assistant Professor
Brianna Martinez is an Assistant Professor with the Hardin-Simmons University Physician Assistant Program. She has clinical experience in Orthopedic Surgery prior to entering education, specializing in Sports Medicine, Total Joint Arthroplasty, and Orthopedic Trauma. She also served as a clinical preceptor for the University Texas Medical Branch for 4 years while living and working in Victoria, TX. She has earned a Bachelor’s of Science degree in Biochemistry from Abilene Christian University and Master’s of Physician Assistant Studies from University Texas Medical Branch in 2015. She is an active member of multiple Physician Assistant organizations, including Physician Assistants in Orthopedic Surgery (PAOS), Texas Academy of Physician Assistants, and American Academy of Physician Assistants. She is married to an HSU alumnus of the Communications and Counseling and Human Development departments. In her spare time, she enjoys serving her local church, reading, exercising, baking and decorating cookies along with her young daughter.
Tenell Zahodnik, MPAS, PA-C
Assistant Professor
Tenell Zahodnik is an assistant professor with the Hardin-Simmons Physician Assistant Program. PA Zahodnik has been an adjunct instructor of Emergency Medicine with the program since 2019 while also serving as the Chief Education APP for the Emergency Department at Hendrick Medical Center. She was recently promoted to the lead APP position at HMC in the Emergency Department. She completed her undergraduate degree at ACU, earning a Bachelor of Science in biology and a minor in business. After graduating from ACU, she worked in marketing/sales for 5 years before deciding to delve into medicine. She graduated PA school from UTMB in 2016. She was at that time recognized as a member of the Pi Alpha Honor Society and Who’s Who Among Students in American Universities and Colleges. She serves on the Education Committee for the Society of Emergency Medicine Physician Assistants (SEMPA) and in 2021, joined the Board of Directors for the organization, where she serves as a Director at Large. She will serve as President-Elect for SEMPA beginning April 2024.
Dr. Kathryn Norton, MD, MBA, FACS
Medical Director, Assistant Professor
Dr. Norton was raised in Abilene, and graduated from Cooper High School in 1990. Her father has cared for patients in the Abilene community since 1976 and it is her goal to carry on the tradition. She attended Schreiner College and graduated with a BA in Biology in 1994. She then attended the medical school at Texas Tech Health Sciences Center in Lubbock and graduated with her Doctor of Medicine degree in 1998. She completed her general surgery residency at Louisiana Health Science Center in Shreveport, LA in 2004. She has continued her education, obtaining an MBA from Texas Tech in 2007. Most recently she has completed Genetics training through the City of Hope. She has a private practice performing many surgeries, but her passion is the treatment and care of breast cancer patients. Dr. Norton is married with 2 wonderful children. She loves the community of Abilene and looks forward to raising her family here and taking care of the people of this community.
Jenni Jamison, MS, MPAS, PA-C
Assistant Professor
Jenni Jamison is an Assistant Professor for the Hardin-Simmons PA Program. She currently serves on the Interprofessional Education Committee for the College of Health Professions and on the Institutional Review Board. She previously worked as a Physician Assistant at Abilene State Supported Living Center, a residential facility for people with IDD. She is a member of the Texas Academy of Physician Assistants and currently serves as the HSU PA Program Faculty Liaison to the TAPA Student Council. She is also a member of the American Academy of Physician Associates and the Association of PAs in Psychiatry. She received bachelor’s and master’s degrees in Psychology from Abilene Christian University. She completed the Master of Physician Assistant Studies Degree from Harding University. She is a singer with Chorus Abilene and currently serves on the Board of Directors. She and her husband are also folk singers and songwriters.
Ashley Hammonds, DD (Hon), MPAS, PA, RT(R)
Assistant Professor
Ashley Hammonds is the Program Director for the Hendrick Medical Center School of Radiography and has served as an Assistant Professor in the Hardin-Simmons University Physician Assistant Program since 2019. He began his career in the United States Air Force as a radiographer, later expanding his expertise through advanced training in Computed Tomography (CT) and Interventional Radiography (IR), where he trained technologists and residents in safe, competent procedures. With more than 20 years of clinical experience and a Bachelor of Applied Arts and Sciences (BAAS) from Lamar University, he went on to earn a Master of Science in Physician Associate Studies from the University of Worcester in England. While there, he served as the lead PA at Hereford Medical Group—a multi-provider practice of over 30 physicians, PAs, and NPs—caring for a patient population exceeding 50,000. He remains registered with the General Medical Council (GMC) as a Physician Associate in the United Kingdom. Since returning to Texas, he has taught a variety of courses at Hardin-Simmons University, including Medical Interview and Physical Examination, Cross-Cultural Medicine, and Radiology. In 2023, he received an honorary Doctor of Divinity for his work in curriculum development and accreditation as a member of the Board of Directors of COTR Theological Seminary. Beyond his professional pursuits, Ashley enjoys playing guitar, studying ancient biblical texts, practicing carpentry, and exploring the world—he has traveled to more than 40 countries. Above all, he cherishes time spent creating memories with his wife, TK, and their three children.
Holly Parker, MMS, MPH, PA-C
Assistant Professor
Holly Parker is an Assistant Professor in the Physician Assistant Program at Hardin-Simmons University. She is a graduate of the Arcadia University Physician Assistant Program in Philadelphia, PA, where she also earned her Master of Public Health (MPH). Holly is currently pursuing a Doctorate in Public Health (DrPH) with a focus on Global Policy and Leadership. After completing her PA education, Holly served as an active-duty Physician Assistant in the United States Air Force for five years, where she developed clinical expertise in Family Medicine and gained international experience. She later transitioned to a position with the Department of Defense, working in both Family Medicine and Aerospace Medicine. Additionally, Holly has clinical experience in Neurology, specializing in Movement Disorders. She is an active member of the Texas Academy of Physician Assistants (TAPA) and the Oklahoma Academy of Physician Assistants (OAPA). Her diverse clinical background, combined with a passion for global health and policy, continues to inform her approach to healthcare and education. In her free time, she enjoys spending time with her husband and their three dogs. She also loves spoiling her nieces and nephews, reading, and exploring new restaurants.Gregory Perry, RPh, PharmD, BCPS-AQID, BCIDP
Assistant Professor
Dr. Greg Perry is an Adjunct Assistant Professor and serves as the instructor for the Pharmacology and Medical Therapeutics I and II courses. He attended Southwestern Oklahoma State University, earning a Bachelor of Science degree in Pharmacy. He graduated from the University of Arkansas for Medical Sciences with a Doctor of Pharmacy degree. He has clinical and pharmacotherapy expertise in several disciplines including critical care (neonate, pediatric and adult), cardiology, infectious diseases, emergency medicine and parenteral nutrition. Dr. Perry is a Board-Certified Pharmacotherapy Specialist and a Board-Certified Infectious Diseases Pharmacist. Dr. Perry has been involved in the implementation of clinical pharmacy services at several health-systems in Texas and Colorado. Dr. Perry is currently the Pharmacy Residency Program Director at United Regional Healthcare System in Wichita Falls, Texas, and he recently became a member of the Society of Infectious Disease Pharmacist Education Committee.
Adjunct Faculty
Jennifer Eames MPAS, DHSc, PA-C
Adjunct Professor
Dr. Jennifer Eames is a part-time Professor for the Physician Assistant Program at Hardin-Simmons University. She obtained her bachelor’s degree from the University of Texas Medical Branch in Physician Assistant Studies and her master’s degree in Physician Assistant Studies from the University of Nebraska with a concentration in Infectious Disease. Dr. Eames also obtained her Doctoral Degree in Health Science from Nova Southeastern University to further her career as a PA educator. She has practiced clinically as a Physician Assistant since 2002 in gastroenterology, family medicine, and infectious disease. Dr. Eames later served as a faculty member, the Admissions Director, and Vice-Chair of the Physician Assistant Program at the University of Texas Medical Branch in Galveston prior to moving to Abilene to originally found the new PA program at Hardin-Simmons University in 2015. As a published author in both educational and professional journals, she is passionate about educating the next generation of physician assistants. She is also passionate about serving her fellow man and has participated in frequent mission work globally including service- learning experiences with her PA and Medical students. Dr. Eames serves on committees and councils at both the state and national level for PAs including being a past president for the Texas Academy of Physician Assistants. Previously, she was one of twelve educators nationally to write the prestigious Physician Assistant Clinical Knowledge Rating Assessment Tool (PACKRAT) exam – given to thousands of PA Students each year across the country and is now on the Board of Directors for the national Physician Assistant Education Association (PAEA). For leisure, she enjoys traveling and spending time with her family.
Samantha Ethridge, MPAS, PA-C
Adjunct Instructor
Samantha Ethridge is a Physician Assistant practicing in Family Medicine at Waco Family Medicine in Waco, TX where she has practiced since graduating from University of Texas Medical Branch Physician Assistant Program in 2014. She attended Baylor University and holds a BS Ed in Health Science Studies and MS Ed in Community Health Education. Before starting PA school, she lived in Southeast Asia as a missionary in Sri Lanka and India working to rebuild villages after the devastating tsunami of 2004, planting churches and helping start businesses for the local people. She enjoys spending time with her husband and 3 children and watching football.
Sammantha Francis, PA
Adjunct Instructor
Sammantha Francis is an Adjunct Instructor for Clinical Elective with the Hardin-Simmons Physician Assistant Program. PA Francis completed her undergraduate degree at Baylor University in Medical Humanities. She was a member of the Equestrian Team and won a Big-12 and National Championship during her time with the team. Sammantha graduated Cum Laude and received the Dr. Gerald-Lage award for excellence in sport and academics. She attended Texas Tech University Health Science center and graduated in 2015. PA Francis has been active in precepting students during her time working as a Hospitalist as well as ER medicine. She was on faculty with University of Colorado Neurosurgery department and enjoyed working with residents and fellows during their training as well. In her spare time, you can find Sammantha hiking, kayaking, or fishing.
Laura Lawrence, MPAS, PA-C
Adjunct Instructor
Laura Lawrence is a Physician Assistant practicing in Internal Medicine and Urgent Care at the Texas City Community Based Outpatient Clinic for Michael E DeBakey Veterans Affairs Medical Center. She is also an adjunct faculty member for the Hardin-Simmons University Physician Assistant Program as the Course Director for Internal Medicine. She graduated from the University of Texas Medical Branch’s Physician Assistant Program in 2006. Mrs. Lawrence has practiced clinically as a PA for over 12 years in gastroenterology and primary care and previously served as a faculty member and Director of Clinical Education for 5 years at UTMB’s PA Program. She attended St. Mary’s University in San Antonio, TX where she obtained a Bachelors of Arts in Biology. Mrs. Lawrence enjoys spending time with her husband of 15 years and their three children and going to church.
Dr. Camille Loftin, DHEd, MPAS, PA-C
Adjunct Instructor
Camille Termini Loftin is a Medical Care Line Physician Assistant at the Texas City Community Based Outpatient Clinic for Michael E DeBakey Veteran Affairs Medical Center. She is also an adjust faculty member for the Hardin-Simmons University Physician Assistant Program as the Course Instructor for Professional Development. She graduated from Texas A&M University in 1989 with a BS in Health Education. She then continued her studies at UTMB and graduated in 1992 from the Physician Assistant Program. She has completed her Doctorate in Health Education at AT Still University. Dr. Loftin worked in the Division of Gastroenterology at UTMB for 4 years, and then went in to private practice in gastroenterology for 14 years before joining the UTMB PAS Department from 2009 to 2017. She has published several abstracts and articles in peer review journals, has numerous poster and oral presentations, and has coordinated several research study protocols. She loves spending time with her husband of 28 years, son, daughter, son-in-law and new grandson Brooks.
Taylor Riggs, MPAS, PA-C
Adjunct Instructor
Taylor Riggs is a Physician Assistant working in Family Medicine at Regence Health Network in Amarillo, TX since 2020. Before joining RHN, she worked for three years at Coastal Health and Wellness/Galveston County Health District in Galveston, Texas. She is passionate about providing high quality medical care to uninsured and underinsured patients. She completed her undergraduate studies at West Texas A&M University in Canyon, Texas. She then received her Masters of Physician Assistant Studies degree from the University of Texas Medical Branch (UTMB) in 2016. In her free time, she enjoys running, hiking, and spending time with her husband, son, and daughter.
Staff
Michelle Crawford
Admissions Coordinator and Administrative Assistant to Program Director
Michelle Crawford is the Admissions Coordinator and Administrative Assistant to the Program Director for the Hardin-Simmons University Physician Assistant Program. Michelle was born in Oklahoma and has lived in Abilene since 2011. She enjoys spending time with her husband and three sons.
Esther Castilleja
Director of Clinical Education
Esther Castilleja is the Director of Clinical Education in the Hardin Simmons Physician Assistant program. She is a native to Abilene and a graduate of Cooper High School. After graduating high school, Esther moved to Dallas/Fort Worth area. She went to Tarrant County College (TCC) and obtained her Associated of Applied Science, with a focus of study in Respiratory Care. Esther became a Registered Respiratory Therapist in 1997 and worked as a Respiratory Care Practitioner for 25 years for a large healthcare organization, in the DFW area. She obtained her Bachelor of Science from the University of Cincinnati in 2018. Her passion was working as an Asthma Educator and as a Pulmonary Rehab specialist, where she worked on educating her patients on disease management and treatment options of chronic lung conditions. Esther also served on the Advisory Board for the Respiratory Care program at TCC for 12 years, where she mentored students and helped develop curriculum. Esther returned to her hometown of Abilene in 2023 and is happy to be home, where she, her husband, and four-legged babies enjoy living out in the country and being closer to family.
Beth Ferguson
Academic Support Coordinator
Beth Ferguson is the Academic Support Coordinator for the Hardin-Simmons University Physician Assistant Program. Beth is from Spur, Texas and has lived in Abilene since the fall of 2019 when she began pursuing her bachelor’s degree in social work at HSU. Beth graduated from HSU in May 2023 and has worked in various capacities at the university during her time as a student and as a graduate. As the PA Program’s Academic Support Coordinator, she incorporates her social work knowledge and skills into how she interacts with her colleagues and the students. Beth enjoys being an active member of Pioneer Drive Baptist Church, spending quality time with her friends and family, and writing poetry.
-
Media Coverage
-
Virtual Tour